Most of us are familiar with the word “bursitis” and have seen it written on MRI or Ultrasound reports. Unfortunately, it is common to blame “bursitis” for the pain and discomfort experienced at different joints.
So, what is bursitis, and why has it become the most hated anatomical structure in the body? Let us review the anatomy first.
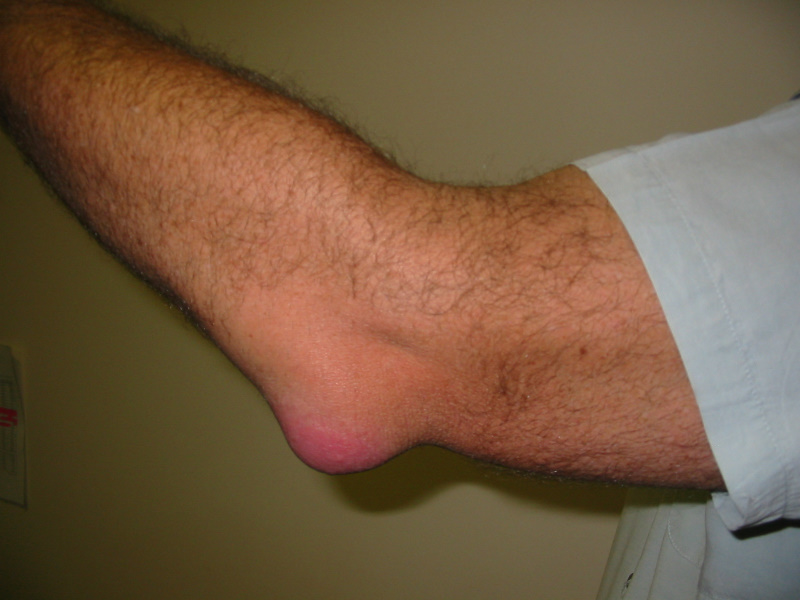
The bursa is a sac of fluid situated between different structures in our body such as bones and tendons. Its role is to reduce friction between these structures, so they may glide smoothly and effortlessly. Bursae are innervated by surrounding nerves which result in increased pain when changes within the bursa occur.
Bursitis occurs when there is increased pressure or friction on the bursa. Most “bursitis” found on imaging, commonly occurs due to overuse or deconditioning of surrounding structures, which causes shearing or compression of the bursa. Our body’s natural response to this, is to increase more fluid to the area to reduce the friction and protect the area, i.e., increase swelling. So, this means we cannot keep blaming the bursae for our pain and consider which structures are overworked so that we may treat that instead.
So, what does this mean when we are diagnosed with the dreaded “bursitis” on images?
- Firstly, we must assess and diagnose the underlying mechanical issue, which is increasing the pressure on our bursae. This must be identified to avoid long-term and/ or recurring pain.
- Secondly, a period of rest from aggravating activities, followed by a tailored strengthening program, to improve the biomechanics and function of the surrounding tissues is vital to reduce the pain and prevent it from returning.
- Finally, reconsider having a cortisone injection without trialing a period of conservative management. Recent evidence has shown that despite cortisone injections reducing pain in the short-term, they do not have a good impact on improving pain and function in the long-term.
So, in summary, next time you see the word “bursitis” on an imaging report, do not panic and automatically assume you will require a cortisone injection. Check in with your physiotherapist to diagnose and treat the underlying cause of compression. As always, if you think this might be an issue for you, book into see one of our physiotherapists to assist with your concerns.
References:
- Speers, C., & Bhogal, G. (2017). Greater trochanteric pain syndrome: a review of diagnosis and management in general practice.
- The International Centre for Allied Health Evidence (2016) Systematic Review of Literature: The Effectiveness of injection of Steroid with or without Local Anaesthetic to the Hip as a form of Interventional Pain Management
- Brukner, P., Khan, K., & Brukner, P. (2012). Brukner & Khan’s clinical sports medicine